Four community-based organizations (CBOs) tackle four different sets of challenges, brought together by a shared vision: a data system that is integrated and responsive to their needs.
The leaders of this quartet of North Carolina-based CBOs—Curamericas Global, Eagle Market Streets Development Corporation (EMSDC), the Institute for Preventive Health Care and Advocacy (IFPHA), and Together for Resilient Youth (TRY)—have consistently found that existing tools for data collection and analysis are driven largely by either the readily available inputs or by the demands of funders and oversight agencies like state governments.
Absent from the design are considerations about what data CBOs truly need, in what format, and for what use to make progress for their clients.
So what would it look like if you came to a common understanding of the problem, and co-created a tool with the community at the center? That was the question they set out to answer, and the result is the Healthy Community Hub (The Hub), a digital resource designed to advance health equity for all.
The Challenge
Public health data are often fragmented and siloed. Health histories from primary care doctors and hospital and acute care records are not always synced, for example. Social determinants of health like housing, employment, exposure to pollutants, or food insecurity are frequently absent altogether, leaving an incomplete picture of a person’s well-being and the risk factors they face for the future.
For me being in healthcare, I’ve seen a lot of tools; some good, some awful, some I hope to never see again. This Healthy Community Hub tool is what healthcare, and especially community-based care, needs.
Kathey Avery, founder of the Institute for Preventive Healthcare & Advocacy
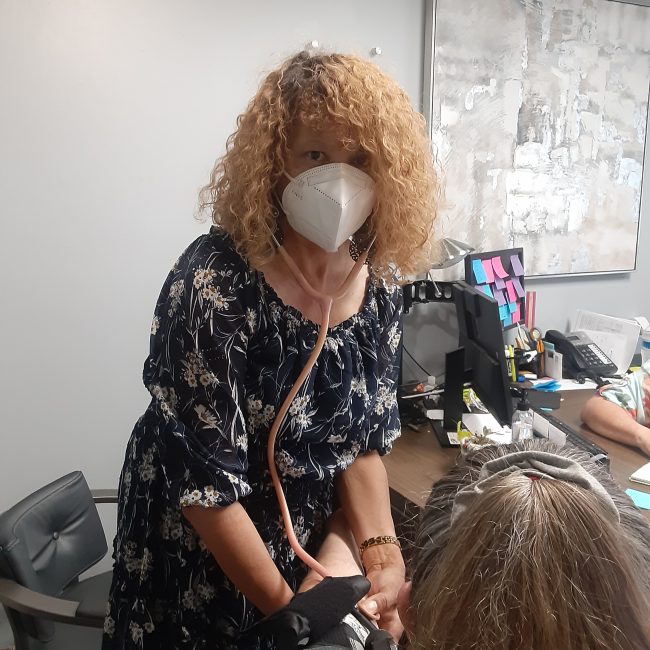
“Social determinants of health—that is part of healthcare. It’s not a sidebar,” said Kathey Avery, founder of the Institute for Preventive Healthcare & Advocacy and a longtime community nurse.
Throughout her career, Avery has used countless data tools but has been consistently unimpressed. Gaps in the data exacerbate systemic racism and deepen health inequities, not to mention the challenges with access to actionable data for the people closest to the work. Data systems, she says, are too often built with the wrong audience in mind, and organizational leaders don’t have the time or capacity to train frontline staff like community health workers in how to leverage data effectively.

“For me being in healthcare, I’ve seen a lot of tools; some good, some awful, some I hope to never see again,” Avery said. “This Healthy Community Hub tool is what healthcare, and especially community-based care, needs.”
Avery and her colleagues had a vision for how the tool should function, informed by feedback and direct experience from community health workers, but they aren’t computer scientists or developers. Building the tool would require technical skills, funding, and ultimately the capacity to consider scaling up so that more organizations like theirs could access usable, transparent community health data in the future.
The Solution
The Healthy Community Hub and Project Resolve, a multi-stakeholder collaboration that brings Microsoft Research’s social science, engineering, and computer science expertise to the table with the North Carolina CBO leaders. Microsoft’s team is building out the tool while also leveraging the partnership to research current community health practices and co-create solutions.
Through the partnership, the Hub is now operational for these four organizations with 42 team members using it and more than 1,883 records created to date. Users have the ability to create client files that give as complete a history as possible, including tags that help to organize and analyze the data by demographic, social determinants of health, medical conditions, or other descriptors. The organizations can also create custom service forms to capture data on services or interventions provided. Requests, like follow-up visits or a recommended treatment plan, can be assigned to specialists. Open requests show up on a dashboard where teams can track workflow.
It starts with cultural humility or humility, period. What is the background of the work you’re doing and if you’re working with underserved populations, what is your capacity to listen to and respect what the community is saying?
Dr. Wanda Boone, founder and CEO of Together for Resilient Youth (TRY)

And built into the tool are reporting features that allow community leaders to filter, manipulate, and understand the data.
“What brought us together was our shared values and vision of what health should look like for everybody, not just the people who already have access,” said Andrew Herrera, executive director of Curamericas Global. “The theory of change – what we’re trying to accomplish – is building up other businesses, other frontline organizations and CBOs to be able to own and measure and customize your data in a dynamic environment as grants or programs get turned on or off.”
Herrera explained that using data tools tied to funding can be problematic. If the funding dries up, you’re left without access or scrambling to find alternative funding sources. Owning the data and directing how it should be collected and used can be a game-changer for leaders on the ground.
“The best solutions come from the community,” said Dr. Wanda Boone, founder and CEO of Together for Resilient Youth (TRY), explaining that they are hungry for data science solutions that leverage existing experience and relationships. “Way before COVID was an issue, we were doing community health work without using that title. Each of us has community members who are equipped to translate information, and community members speak to these community influencers and thereby become ambassadors of health.”
The team agrees that a foundation of trust is essential. Trust-building is time-consuming, but it’s the only way to get accurate information about the challenges, risks, and opportunities for health equity in communities. Without trust, the same mistakes will keep happening in making assumptions about what people need and how best to deliver care.
For other organizations or states looking to embark on similar work, that’s a key piece of advice, says Dr. Boone, and one that funders and boards of directors should keep in mind as they look for results.
“For me, it starts with cultural humility or humility, period. What is the background of the work you’re doing and if you’re working with underserved populations, what is your capacity to listen to what the community is saying and respect what the community is saying?” she said.
The Takeaway
Mary Gray, the senior principal researcher for Microsoft Research, says Project Resolve has reinforced the importance of community-led design and building trust before offering solutions, however well-intended. It has been an eye-opening experience for her and she hopes it will be a humbling one for her colleagues in tech.
She recalls one point of tension between the CBO leaders on the ground and the engineering team building the tool. Community health workers spend their time in the field, meeting people where they are and making house calls to remove barriers to care access. They wanted the ability to print records or service forms, and the engineers backing up the tool couldn’t understand why the print function was a priority.
“I am just still so surprised by how hard it is to have engineering yield and listen to what people might need. There’s no muscle in tech for doing this work,” Gray said. “People in communities already have solutions for what they’re doing, and I’m constantly surprised at how hard it is for engineering to start from the solutions people already have in their lives.”
Those moments of friction will continue, but the Healthy Community Hub and Project Resolve teams are committed to working through them. In the near term, they want to increase the number of users and increase the amount of time users are spending with the tool. They want to add new functionality, like a calendar feature and other elements that community health workers say they would find useful. Improving data security is an ongoing priority. For health workers on the ground, though, having those materials handy when they’re on the road and in communities helps make their work easier and their recommended interventions more effective.
In the long term, the team believes they have a product that makes a difference. A product that Stephanie Swepson Twitty, CEO of Eagle Market Streets Development Corporation, believes has the power to improve health equity and strengthen CBOs around the country and globally.
“All of us are in significant need of data to inform our work,” she said. “I’m looking at a business model that can be replicated across the state, across the nation, whereby community tech teams come together and are able to respond to data needs of the community.”
